Fertility Problems
Human Reproduction
1. The menstrual cycle
2. Fertility and female age
3. Sperm production
1. The menstrual cycle
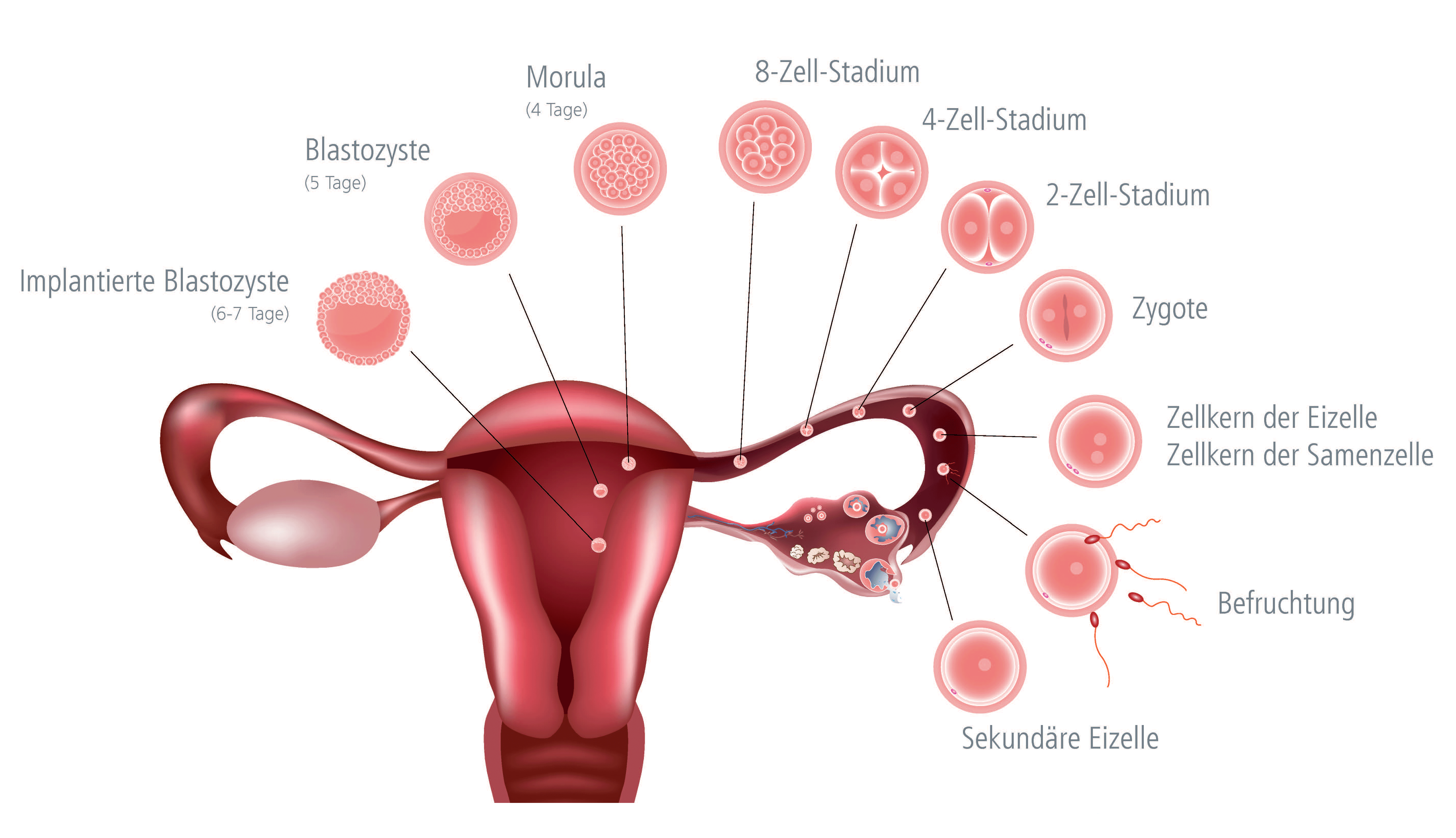
A woman's cycle starts on the first day of her period. Every month an egg matures in one of the ovaries. The egg (oocyte) develops within a follicle. Already, during the previous cycle, the ovaries start preparing the next batch of follicles (on average 10-12) for ovulation taking place the following month. Usually, only one follicle reaches full maturity and is ovulated, while the others degenerate.
A mature ovarian follicle is a fluid-filled vesicle of about 2 cm in size. The wall of the follicle serves as a protective casing around the ovum. The follicle reaches its maximum size in the middle of the menstrual cycle. Ovulation typically occurs around day 14. When the follicle ruptures, the ovum and follicular fluid are released into the fallopian tube (ovulation). Hair-like structures (cilia) lining the inside walls of the fallopian (uterine) tubes along with finely-tuned muscular contractions help move the egg towards the uterus.
│ © 2022 Shutterstock/Next Fertility IVF Prof. Zech • Member of Next Clinics
If sexual intercourse occurs around the time of ovulation, the ejaculated sperm enter the vagina and travel through the cervix and uterus up to the upper portion of the fallopian tube where the oocyte is waiting for a single sperm to fertilize it.
The fertilized oocyte, now referred to as an embryo, already begins to undergo a series of cell divisions while still in the fallopian tube. On average about day 5 after ovulation, the embryo reaches the uterine cavity where it starts implanting itself in the endometrium (uterine lining).
During each menstrual cycle, the uterus grows a new lining (endometrium) to be well prepared for potential implantation of an embryo. As the ovarian follicles develop, they produce the hormone "estrogen". The larger the follicles get, the higher the increase in estrogen levels. This hormone is responsible for the buildup of the uterine mucosa on the days leading up to ovulation.
The so-called yellow body (corpus luteum) forms from the remnants of the follicle left behind after ovulation (the corpus luteum is a temporary endocrine structure resulting from proliferation of the granulosa cells that line the follicular walls). The corpus luteum secretes "progesterone", which is a hormone responsible for preparing the uterine lining (endometrium) for the implantation of an embryo.
Once implantation occurs, the embryo begins to form and secrete hCG (hCG is a hormone the body produces during pregnancy. Chemical pregnancy tests look for the presence of human chorionic gonadotropin (hcG) in the blood or urine).
In the first 10-12 days following implantation, the embryo is still very small and therefore produces hCG levels that fall below the measurable limit. But as it grows, the hCG levels rise and they send a signal to the corpus luteum to keep producing progesterone, which, in turn is essential for maintaining the uterine lining (instead of shedding it with the onset of menstrual bleeding).
Corpus luteum insufficiency
If embryo implantation fails to occur, progesterone levels remain low in the absence of signals sent out by a developing embryo. The corpus luteum starts to wither and the lining of the uterus (endometrium) breaks down and is shed, marking the beginning of a new cycle. The onset of menstrual bleeding can be seen as the starting signal for a new cycle. All these processes are controlled by a highly complex mechanism regulating the interactions between the ovaries, the pituitary gland (hypophysis) and the hypothalamus of the brain.
2. Fertility and female age
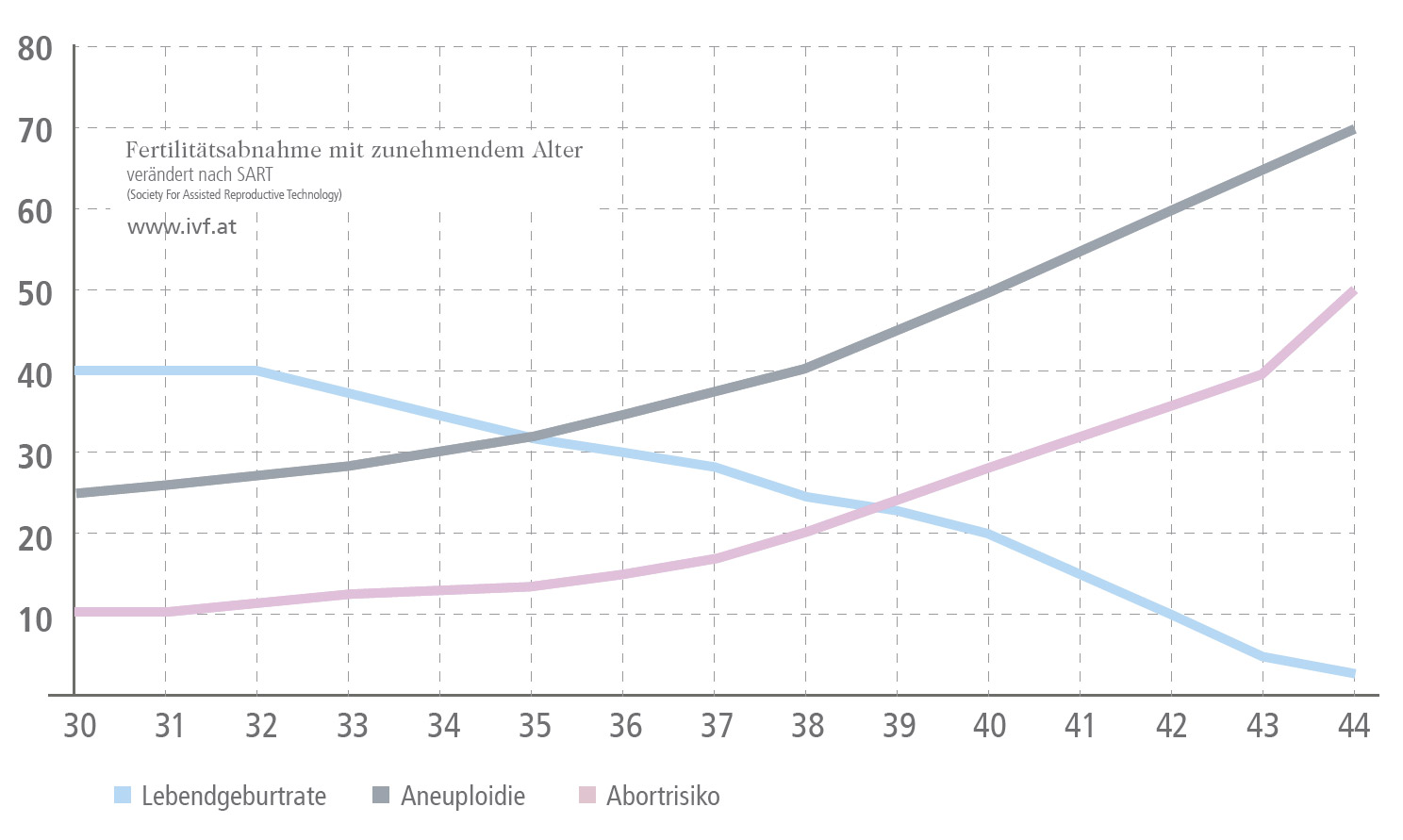
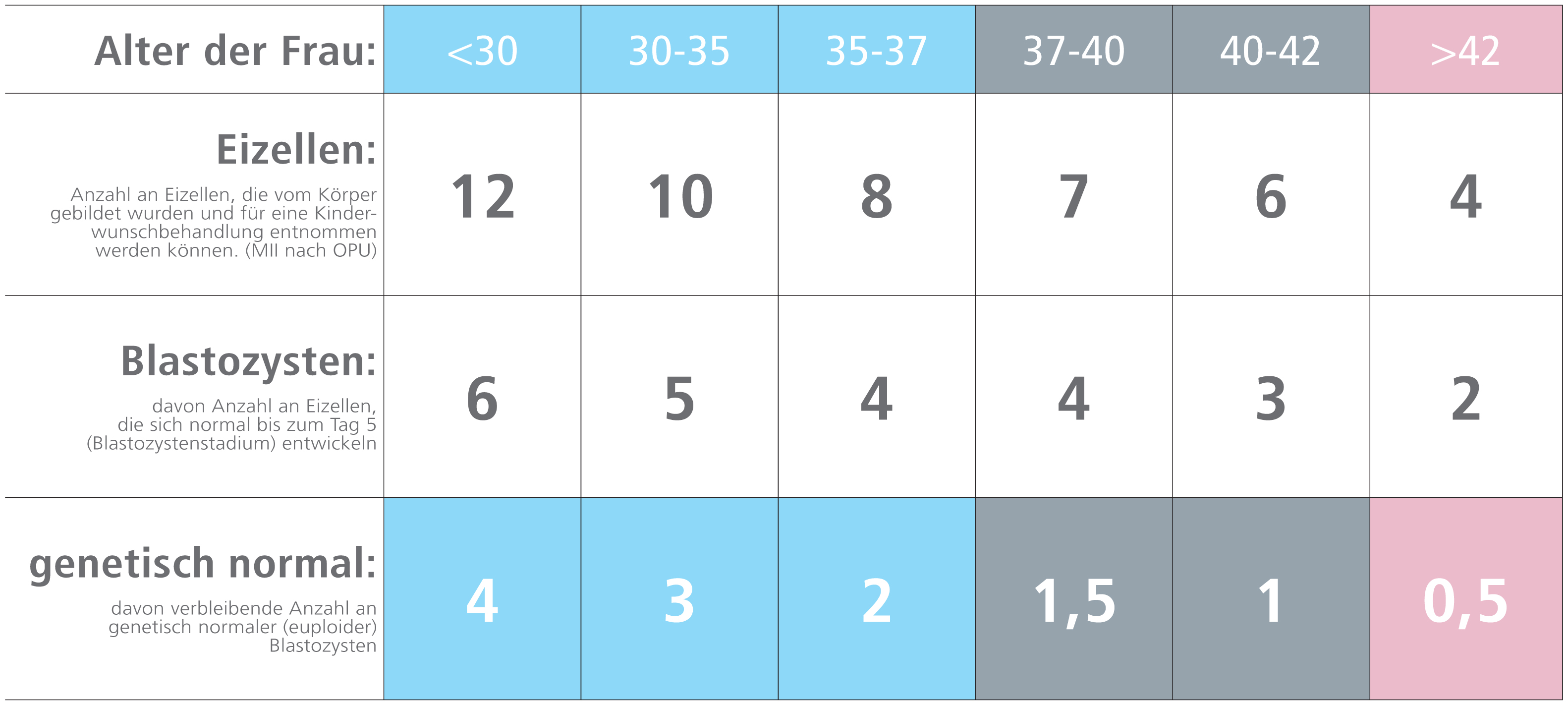
A woman's "natural" fertility peaks between the age of 25 and 35. Female fertility declines from about the age of 38. Beyond age 43, the chances of conceiving naturally are considerably reduced. The quantity and quality of the oocytes have the most impact on female reproductive capacity. As women age, they are faced with a decline in both the quantity and qualitiy of their oocytes.
With advancing maternal age, there is another issue that plays a crucial role: numerical chromosomal abnormalities are more likely to develop in the oocytes of older women (aneuploidy - the presence of an abnormal number of chromosomes in the egg cell (above or below the normal chromosome number). The fertilization of an affected oocyte often results in poor embryo development and implantation failure. If, however, such pregnancies do occur, they often end in spontaneous miscarriage, but in rare cases can lead to the birth of a child suffering from a genetic disorder.
Age-related decline in fertility
│ © 2022 Next Fertility IVF Prof. Zech • Member of Next Clinics
Number of oocytes and their age-related potential for development
│ © 2022 Next Fertility IVF Prof. Zech • Member of Next Clinics
3. Sperm production
Healthy young men produce around 100 million sperm every day. The development of sperm takes place in the testicles under the influence of two essential hormones, namely LH and FSH. These hormones are secreted by the pituitary gland (hypophysis). FSH plays a pivotal role in the maturation of the spermatozoa inside the seminiferous tubules. LH triggers the production of testosterone which is the most important androgen and plays a key role in the development of male reproductive tissues and spermatogenesis. In the past decades, a sperm count of more than 50 million sperm/ml was considered normal. More recent WHO criteria state that a sperm density above 15 million sperm/ml of semen is normal. This clearly indicates the dramatic drop in sperm counts over the past years. About 1200 sperm cells per second are produced in the testes. It takes about 3 months for a spermatozoon to be formed and get ejaculated from the testis. Following drug treatment or other therapeutic options, an improvement in semen quality (or better IMSI-results) can be expected after this lapse of time.
Couples who want to conceive but still have not become pregnant after one year of having regular intercourse without using any form of contraception should seek medical help to identify the underlying reasons.